A ‘good’ myth (or a very ‘bad’ one, choose your PoV…), such as the idea the we only use 10% of our brain thrives in the confusion about how much evidence there is against it and how we obtain this evidence. In our case, we’ve seen how this wasn’t helped by early and well known proponents of localisation, who muddied the water with dodgy methods and idiosyncratic lists of faculties populating the cognitive landscape (Part 2).
Today’s topic is the growth of a more principled and systematic approach to exploring relationships between brain damage and behavioural and cognitive alterations. These days, for many patients, we can discover (or discount) physical causes of behavioural problems ‘in real time’ with brain scans. This may blind us to the fact that this is a relatively recent development, indeed only became possible in the later decades of the 20th century. Previously, in almost all cases the only way to confirm the inference of physical damage was by autopsy – often with a large gap in time between the onset of symptoms and the point when patient died. This means that finding associations required observation and record keeping over years or even decades. In an age of national health services and record keeping technologies this may not sound like much. But in the 19th Century, the creation of organisations with the will and the capacity to do so combined with the clinical insight to see what this set might tell you, was itself an innovation.
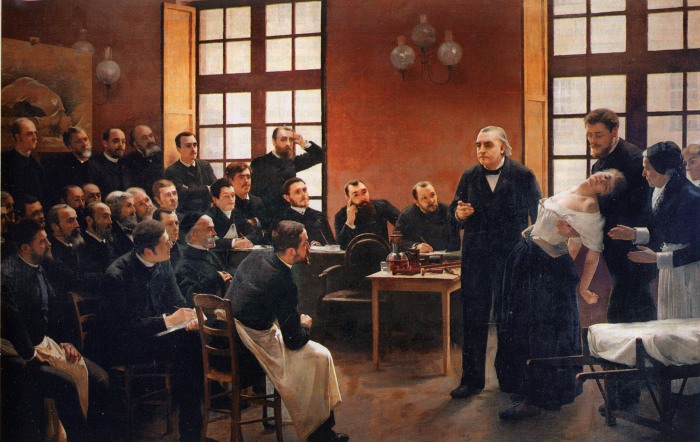
If the birth of neurology and what would become known as the ‘anatomo-clinical’ method can be associated with a particular place and person, it would be Hôpital universitaire la Pitié-Salpêtrière at Paris, and Jean Martin Charcot (1825-1893) who worked and taught there for 33 years [1]. Though not the method’s inventor, Charcot developed it further through the close, regular and ongoing observation of patients, followed-up over years, connecting behavioural and physiological abnormalities. Charcot, his students and collaborators better described, diagnostically differentiated and sometimes found treatments for a range of conditions. Notably, this includes Multiple Sclerosis and it’s destruction of the fatty material (myelin) that insulates axons, but also Parkinson’s Disease, amyotrophic lateral sclerosis, and Tourette’s syndrome, among others. By careful classification of in vivo symptoms and post-mortem pathology, Charcot had shown it was possible combine the two sets of information to map out the space of neurological impacts. One could learn to differentiate and recognise signs of damage to the brain versus the spinal cord, or nerve versus muscle damage, by observing the cluster of symptoms presented by a patient.

While phrenology had earned localisationism a bad name in some quarters, others were not afraid to posit associations between certain kinds of damage and certain kinds of deficit. For example, the work of Paul Broca (1824-1880), a respected physician who in 1861 reported on the autopsy of a patient, Louis Victor Leborgne [1,2]. Lebourgne had first been admitted to the hospital twenty years before this death due an abrupt loss of the ability to speak, even though he continued to understand what was said to him. The only word he could say was ‘Tan’. After Lebourgne’s death, autopsy showed a fluid filled hole in the posterior part of the left frontal lobe. Following (and acknowledging) earlier work by Jean- Baptiste Bouillaud Bouillaud and Ernest Aubertin Broca identified this region as a consistent site of damage in patients with what he called ‘aphémie’, or aphasia. The fact that this association between aphasia and posterior frontal damage often – though not always – implicated the left frontal lobe was a puzzle, especially given prevailing ideas about equipotentiality in brain function. Linking the facts that the left side of the brain controls the right side of the body, and that most people are right handers, Broca proposed the left hemisphere was ‘dominant’ over the right. Indeed, hemispheric dominance for language is more often modified in left-handers. By suggesting that this dominance could be modified in some situations, Broca also offered an explanation why some patients with damage like Lebourgne’s retained fluent speech. Thanks perhaps to Broca’s stature, and the fact that he took care to distance himself and his findings from phrenology, this region has become known as Broca’s area.

Another important insight in the development of neurology, this time in the UK, as well as for burgeoning ideas about brain organisation is the recognition by Hughlings Jackson (1835- 1811) [1], that the way epileptic convulsions manifest is not just random, but often includes certain muscle groups in a particular order. This informed not only his classifications of epilepsy, from which modern systems of classification developed, but also a hypothesis about the organisation of motor cortex. His suggestion (essentially correct), was that the motor cortex was set out in a way that mimicked the organisation of the body, which we call somatotopic (‘somato-’ referring to the body). Jackson also became interested in aphasia through working with people who had suffered strokes. He came to be in broad agreement with Broca that the two hemispheres differed in function, and impacts to the ability to produce speech disturbances were likely to be caused by left-sided damage. However, unlike Broca he argued that some language function was native to both hemispheres, based on experience with patients with right-side damage whose speech was nonetheless impacted. Because this impact seemed to manifest in a different way to left-sided damage he proposed the right hemisphere specialized in emotional and involuntary expressions and in recognising objects and people, with the left specialising in propositional/intellectual speech.
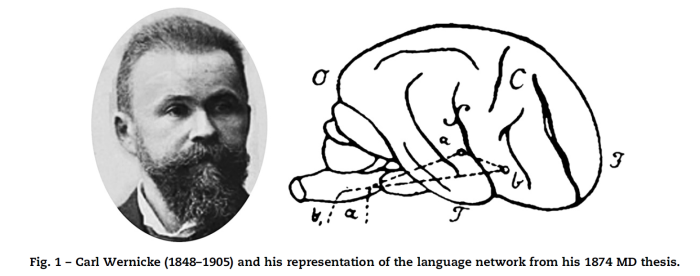
Picking up up these threads and adding his own contributions in a model of language in the brain, is another important name Carl Wernicke (1848-1905). He characterised another type of Aphasia where speech comprehension was very poor but the production of speech was fluent, in the sense that people affected by it don’t have difficulty producing words and sentences, though their productions are made up of ‘nonsense’ words and inappropriate expressions. This is in contrast to the intact understanding but production difficulties in the patients described by Broca. The two types have become known as Wernicke’s (or receptive / sensory) aphasia, and Broca’s (or expressive) aphasia, respectively. The type of aphasia that Wernicke recognised is associated with damage to the left temporal lobe.
In fully recognising that Broca’s aphasia represented a problem in producing speech, while the patients he was describing exhibited a problem with comprehension, Wernicke made another major contribution in proposing a model of language processing in the brain that was remarkably accurate for its time. He suggested that the temporal region represented a ‘sound field’ that received input from the ears and ‘understood’ it by comparing the sensory input to a store of sounds in memory, which could be forwarded to frontal regions like Broca’s, who could form a response via the controlling the physical speech apparatus. Importantly, this model made predictions, the sign of a maturing theoretical construct. It implied a connection existed between the two regions in the temporal and frontal lobes that had been associated with language. Wernicke hypothesized that damage to this connection would leave comprehension and production intact, but impact the passing of information between regions, manifesting, for example, as a difficulty in repetition of words spoken by others. This type of aphasia, known as conduction aphasia, does in fact exist.
The seminal discoveries and concepts at the foundation of neurology and neuroscience occurred in the absence of modern technologies. They were made by early neurologists, often based on studies of individuals or groups affected by neurological pathology. They came from the close observation of patients, the recognition of clusters in symptoms, and the imagination to consider what this might all telling us about the damaged organ of the brain. We’ve seen how this relates to the history of multiple sclerosis and epilepsy, and the developing understanding of language in the brain presents a useful ‘arc’. These aren’t the only domain where accounts of small numbers of individual had a large impact on our thinking about thinking. For example, we’ve discussed Henry Molaison (Patient H.M.) and others and their importance in the context of memory, not to mention neuroethics & CJ Cherryh’s Downbelow Station. Eagled-eyed readers who know their stuff may have noticed a major absence in the person of Phineas Gage, because I’m saving his story for a later post. These cases, and the functional localisation that these singular individuals led their physicians to suspect, had – and continue to have – a huge influence on our our ideas on about functional localisation.
While we may localise the damage that makes a man speechless, we do not localise language. It will reside in the whole brain.
Hughlings Jackson, in [1]
It should be noted, of course, that this kind of ‘cortical cartography’ is only the beginning of understanding, not it’s endpoint. For example, despite his contributions, Hughlings Jackson was not a strict localisationist, while also not being wholly committed to equipotentiality [1]. He squared this circle via an analogy to the retina of the eye (as featured here & here), likening the broad capacity of the whole retina to respond to light to the broad and likely distributed contributions necessary to language. In this view regions with ‘localized’ function such as the putative Broca’s area are comparable to the fovea, the region of high acuity at the centre of the retina. Without nuance, talking only in terms of ‘a brain centre for x’ can be as equally as dodgy a trope as 10%urBrain. A deeper understanding of the associations between observed behaviour, neuronal ‘activity’ and brain anatomy and connectivity is a major motivator of brain science. As I hope I have shown, this was the case from the early days of neurology. It is also the case now, as modern technology provides new ways to answer these questions that were not available to our forbears. But that’s a story for another time…
This post is part of a series. Other posts can be found here:
Part One – Introduction: why the trope is bad science and, even worse, bad fiction.
Part Two – Early misteps with phrenology
REFERENCES
[1] Andrew P. Wickens, A History of the Brain: From Stone Age Surgery to Modern Neuroscience, 2014, Psychology Press
[2] M. T de Schotten et al 2015. From Phineas Gage and Monsieur Leborgne to H.M.: Revisiting Disconnection Syndromes. Cerebral Cortex, 1–16
[3] Marco Catania & Marsel Mesulamb 2008. The arcuate fasciculus and the disconnection theme in language and aphasia: History and current state. Cortex, 44, 953-961

7 thoughts on “Your Brain Through…History: the nonsense “you use 10% of your brain’’ trope that won’t die, and why (3)”